According to research, as many as 47.8% of women of reproductive age (i.e. those who are actively menstruating) experience symptoms of premenstrual syndrome, or PMS. Of this percentage, around 20% “experience symptoms severe enough to disrupt their daily activities, and the remaining have mild to moderate symptoms”1.
With this in mind, it’s unsurprising that many look for support and supplemental options to reduce or manage symptoms. In this guide, we’ll take you through everything you need to know about premenstrual syndrome, including what the best PMS supplements are…
What is PMS?
PMS has regularly been mocked in the media and popular culture, but it’s a real thing. Loads of us have experienced drastic mood swings, cramping, and a whole host of symptoms in the days leading up to a period.
So, to kick things off, let’s begin with a medical definition.
Premenstrual syndrome, as defined by the NHS, is “the name for the symptoms women can experience in the weeks before their period”2. There are a wide range of symptoms (as we’ll explore in more depth below) and these do not affect every person equally. What is most important to note is that PMS can impact anyone who has periods with varying severity, and can affect regular daily life.
But what actually is it? To understand that, we should first look at the menstrual cycle as a whole.
The menstrual cycle
Biologically speaking, the menstrual cycle most directly involves two different areas of the female reproductive system: the ovary and the endometrium3 (aka the uterine lining).
Each of these areas go through different phases. In the ovary, these are the (somewhat) more well-known follicular, ovulation, and luteal phases. In the endometrium, you have the proliferative, secretory, and menstrual phases. However, these are not isolated from each other within the wider menstrual cycle; they happen concurrently as part of the overall reproductive system.

Follicular and proliferative phases
The follicular phase begins on the first day of menstruation, and lasts to the start of ovulation4 (which is usually day 14 of the cycle). However, for people with longer or shorter cycles, the follicular phase will vary in length.
In simple terms, the follicular phase is where the new oocyte (or ovum, or egg) is being prepared for ovulation and potential reproduction.
Within the ovary are thousands of “small, fluid-filled sacs” called ovarian follicles that contain one immature egg5 each. Hormone production in the brain at the beginning of the menstrual cycle triggers follicles to start maturing. Towards the end of this phase, one follicle per cycle is deemed dominant; eventually breaking open to release the ovum ready for ovulation.
Did you know?: oestrogen levels reach two peaks during menstruation: one of which is late in the follicular phase, just before it sharply declines after ovulation6. The other is midway through the luteal phase.
While the follicles are maturing in the ovary, the uterus is also beginning to prepare for potential pregnancy. This is called the proliferative phase.
During this phase, the innermost lining of the endometrium, which is itself the innermost lining of the uterus, reaches its maximum thickness. Blood vessels around the endometrium also elongate to increase blood flow and accommodate for the thicker layer. The cervix also dilates and releases a thin discharge designed to decrease the acidity of the vagina (to make it a more hospitable environment for sperm)7. Effectively, the uterus is setting itself up as the ideal habitat for a fertilised egg.
Ovulation
Strictly speaking, ovulation occurs when the mature egg is freed during the rupture of the dominant follicle8. The new ovum is taken up by the fallopian tubes, where it waits to be potentially fertilised by sperm.
The days shortly before, and just after, ovulation are when you are at your most fertile - particularly as sperm can survive a few days within the body.
Did you know?: the fallopian tubes are not directly connected to the ovaries. Instead, thin tendril-like projections called fimbriae are there to usher the egg into the fallopian tubes.
Luteal and secretory phases
Once the egg has been released, the next stage of the menstrual cycle is effectively a waiting game. There are two options here; either the egg is fertilised, in which case the body prepares for pregnancy; or it isn’t, and the body begins the cycle anew.
The luteal phase begins when ovulation finishes, and lasts until pregnancy or menstruation. Unlike the follicular phase, the luteal phase is relatively consistent for each individual, and usually lasts around 14 days9.
During the luteal phase, the burst follicle (that released the mature egg), develops into the corpus luteum. The corpus luteum is an essential part of the cycle, as it releases progesterone. Progesterone is a key hormone for maintaining the endometrium and ensuring the uterus can be a healthy environment for a zygote (fertilised egg) to implant and become a foetus10. From here, there are two possibilities11:
-
If conception occurs, the fertilised egg releases HCG, or human chorionic gonadotropin. This preserves the corpus luteum, and it will continue to release progesterone until around week 12 (the end of the first trimester); after which the placenta is able to release enough progesterone to support the pregnancy.
-
If the egg remains unfertilised, the corpus luteum breaks down, which happens around 10 days after ovulation. Without the release of progesterone, the endometrial lining decays, and your body sheds it (basically becoming what you’re more familiar with as a period).
Did you know?: the luteal phase can also be referred to as the secretory phase due to the secretion of progesterone and other hormones from the corpus luteum, in addition to fluid secreted by the endometrium.
Menstruation
Periods, or menstrual fluid, contain blood, the shed endometrial cells, some vaginal secretions, and various other enzymes and biological chemicals12. Menstruation technically happens at the beginning of the follicular phase - usually lasting between 3-5 days, but can be up to 8 days. Clots are less likely, unless your flow is very heavy.
The average menstrual cycle
The average menstrual cycle is around 28 days, but it’s also completely normal to have longer or shorter cycles (between 21-35 days). In the UK, the average age to start a period is 12, while the average age for menopause (where periods stop) is 5113.
This means that the average woman will experience around 480 periods in her reproductive life! However, this figure will be lower if she experiences a pregnancy, as ovulation (and therefore periods) stop.
Did you know?: on average, you lose between 20-90ml of blood during a period14 - but this can be more if you experience a heavier flow.
Where does PMS fit in?
To conclude our whistlestop tour through the menstrual cycle, let’s look at how PMS fits in.
PMS occurs during the luteal phase, between ovulation and menstruation. To put it simply, this is a time when the body is experiencing a relatively rapid influx of hormonal changes, from increased progesterone to fluctuating oestrogen, all of which has an impact on regular emotional, behavioural, and physical health.
Studies have indicated that PMS mood disorders (see below) are linked to fluctuating oestrogen levels, primarily through oestrogen-serotonin regulation15. Decreased progesterone in the late luteal phase has also been linked to disrupted and disordered sleep16.
What are the symptoms of PMS?
Premenstrual syndrome presents itself in a wide range of symptoms, and you may experience some or all of these to various degrees. You may also not experience the same symptoms every cycle, or at the same level.
Basically, PMS symptoms really depend on the individual, and will change a lot. With that being said, the most common symptoms of PMS are17:
-
Mood swings, such as increased irritability.
-
Low mood and/or increased feelings of anxiety.
-
Headaches.
-
Tiredness and/or trouble sleeping.
-
Bloating and cramping.
-
Tenderness in your breasts.
-
Appetite changes and specific food cravings.
-
An increase in spots, greasy skin, and greasy hair.
These are all mild to moderate symptoms, and can be managed with lifestyle, diet, and supplemental support.
More severe symptoms of PMS are known as PMDD, or premenstrual dysphoric disorder. These can be incredibly intense, and have a bigger impact on your daily life and routine. PMDD symptoms can be physical or mental, and include18:
-
Headaches, joint and muscle pain.
-
Disordered eating.
-
Insomnia and/or trouble sleeping.
-
Increased feelings of depression, suicidal ideation, anger, and anxiety.
The best supplements for PMS
Let’s be clear: PMS sucks. It’s not the most scientific way to put it, but it is the simplest. The hormonal changes you experience in the lead up to your period can sometimes make you feel crazy - and it’s worth saying that it’s not your fault.
However, there are some lifestyle changes you can do to help:
-
Eat a balanced, healthy diet. If you struggle with bloating, you might want to switch your diet to eating smaller meals more frequently to be more comfortable.
-
Exercise regularly. Even if you don’t feel like it, exercise can be a huge mood booster, and help combat increased feelings of anxiety and low mood.
-
Try to get plenty of sleep. Changes in your hormone levels can impact your sleep, so where possible, try and stick to a regular sleep hygiene routine to encourage a good night’s rest.
-
Find ways to reduce stress. Journaling, yoga, and meditation are all valid forms to help you process and manage your stress levels in the lead up to your period.
-
Take painkillers. Over the counter painkillers like paracetamol and ibuprofen can help ease pain and soreness.
Top tip: if you find that your symptoms are impacting your daily life a lot, try keeping a journal for a few cycles. This will help during a GP appointment to find the best solutions for you.
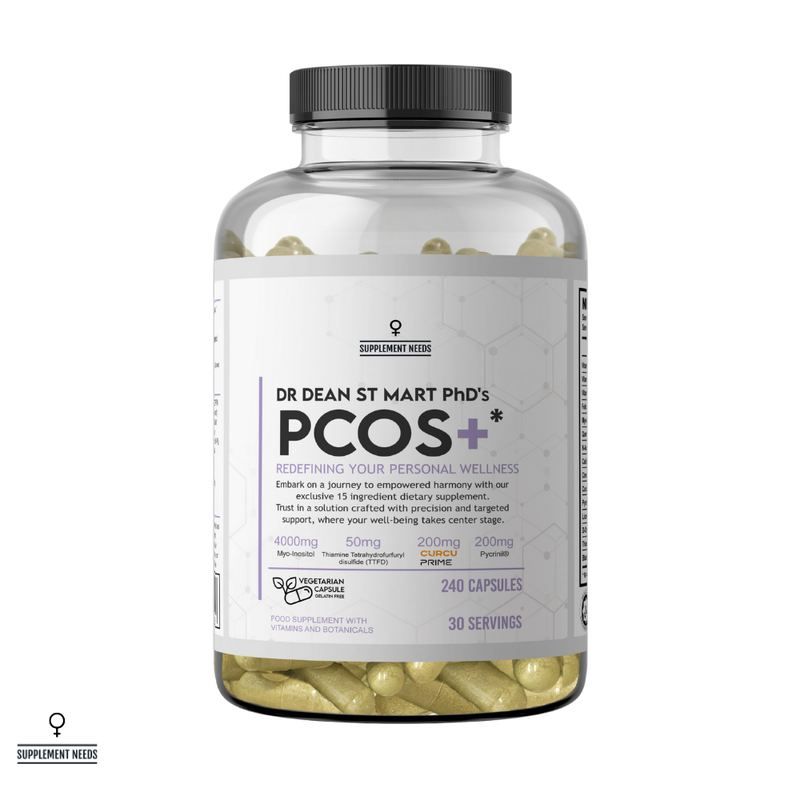
Alongside certain lifestyle changes, you might want to consider adding a supplement to your diet. There are a range of ingredients that may help to ease your symptoms, or you can choose a specifically-designed supplement to include in your diet - like Supplement Needs’ PMS+ capsules.
In the section below, we’ve picked out some of the key ingredients that can be beneficial to help you manage PMS symptoms and support your health…
B Vitamins

B Vitamins are important for a lot of bodily functions, including but not limited to obtaining energy from food, storing it in the body, and helping produce healthy red blood cells19. When it comes to alleviating PMS symptoms, these can come in handy, especially:
-
Vitamin B6: some studies have shown that Vitamin B6 can help to alleviate and reduce PMS symptoms - potentially through serotonin production20.
-
Vitamin B12: evidence suggests that when taken in conjunction with fatty acids, like omega-3, B12 can help to alleviate menstrual pain21.
-
Vitamin B1: Vitamin B1 may increase the release of endorphins, and release ATP, helping provide energy and stimulate sleep22.
Magnesium bisglycinate

Magnesium is one of the essential minerals your body needs to function. It plays a role in energy extraction, as well as ensuring your parathyroid glands work properly (these glands produce important hormones for bone health)23.
According to research, supplementing with magnesium can help to prevent menstrual migraines, dysmenorrhea (which is the medical word for menstrual cramps), and PMS symptoms24.
At Supplement Needs, our PMS+ contains magnesium bisglycinate. This is a more bioavailable form, which means your body finds it easier to absorb. To learn more, we’ve put together a guide on What are the Potential Benefits of Magnesium Bisglycinate?
Vitamin D

Vitamin D is one of the few dietary components that you don’t fully get from your actual diet. Instead, your body produces Vitamin D with exposure to UV light - which is why it’s much easier to get enough in the summer. In the UK, it’s actually recommended that adults supplement with Vitamin D in the winter to reduce the chances of developing a deficiency25.
While more research is still needed, there are studies that support Vitamin D supplementation for PMS symptom management. Vitamin D is essential for the female reproductive system more widely, and has been linked to reducing cramps, inflammation, and PMS-related mood disorders26.
Ashwagandha

Ashwagandha has had a presence in traditional medicinal practices for millennia. In Ayurvedic medicine (originating from India and Nepal), ashwagandha has been used to treat everything from joint inflammation to insomnia.
As a PMS treatment, studies have shown ashwagandha had a positive impact on mood, reducing stress, anxiety, depressive symptoms and irritability. It has also been shown to help with poor sleep, and bloating before menstruation27.
Learn more about ashwagandha and its long history in traditional medicine in our guide to What is Ashwagandha & What Does it Do?
Inositol

Inositol is a naturally produced sugar found in the body. It’s largely responsible for helping your cells maintain their structure (via the cell membrane)28. Alongside this important function, it’s also been linked to improving PCOS (polycystic ovary syndrome) and PMS.
How? There is promising research to suggest that inositol can help to improve symptoms of depression by helping to balance serotonin and dopamine in the brain29. This was shown to be particularly effective in participants with PMS, suggesting it may be a good treatment for the psychological symptoms30.
Ginger

Much like ashwagandha, ginger has a long history as a traditional medicine - being used to treat arthritis, nausea, and other common mild maladies.
In terms of PMS, this has stood it in good stead as a way to manage or reduce PMS symptoms. According to early research, ginger has been shown to reduce nausea, PMS-related joint and muscle pain, menstrual headaches, and dysmenorrhea (both back and abdominal pain)31.
While the exact manner is unconfirmed, it is thought that ginger inhibits the production of prostaglandins (which are hormones that affect uterine contractions, pain, and inflammation)32.
Ginkgo biloba
Ginkgo biloba is actually one of the most commonly used herbal supplements in the world33. Prized for its neuroprotective, antioxidative, and vasodilatory properties, it has been used to treat a wide range of conditions, including cognitive impairment, cardiovascular disease, and various psychiatric disorders (to name but a few).
As a PMS treatment, ginkgo biloba has been linked to improving mood and behavioural symptoms, such as depression. It’s also been shown to increase blood circulation, reduce inflammation, and regulate stress34.
Vitex agnus castus
Vitex agnus castus, or chasteberry, is a fruit from the chaste tree (so-called as it was believed to be an anaphrodisiac, or libido reducer35 in men).
As a way to manage PMS symptoms, vitex agnus castus has been linked to reducing breast pain or tenderness, and alleviating low moods, headaches, and anger36.
Lemon balm
Lemon balm, or melissa officinalis, is “an oily extract”37 taken from the leaves of the melissa officinalis plant - a flowering shrub common in the eastern Mediterranean and western Asia.
Throughout traditional medicine, it’s been used to treat menstrual irregularities. More recent research has shown that it can help reduce the severity of PMS-related fatigue, lethargy, anxiety, and depression - importantly without increasing the severity of menstrual bleeding (making periods heavier)38.
Zinc monomethionine
Zinc is another essential mineral that has shown potential as a way to reduce PMS symptoms. According to research, zinc supplementation improved mental health scores of participants, suggesting it can help to reduce emotional symptoms for better quality of life39.
Choosing the best supplements for PMS
Now that you know the key ingredients you should be looking for, what about choosing the best supplements for the job?
-
👩 Designed for women: a lot of the ingredients we’ve mentioned are in a range of supplements. But, when it comes to managing PMS symptoms, generic isn’t going to cut it. That’s why you should always look for PMS supplements that are specifically formulated with female needs in mind. Here at Supplement Needs for example, we understand that you need tailored supplements explicitly to meet the needs of the female body - which is why we’ve created our Female Needs collection.
-
🔍 Non-generic, transparent ingredients: we’ve already said it, but when it comes to supplements, generic is not the one. Always look out for trademarked, propriety, and well-researched ingredients to ensure you’re getting the best. At Supplement Needs, we’ve even gone one step further. Not only can you find the exact nutritional content of your supplement, but also which part of the plant, or form they are in. Full ingredient transparency - guaranteed.
-
💧 Enhanced bioavailability: to get the most out of each dose, look for supplements that use the most bioavailable form. As we mentioned above, our PMS+ supplements use magnesium bisglycinate and zinc monomethionine for maximum absorption. By chelating supplements, your body finds it easier to absorb the active ingredients.
-
Chelation is basically a buddy system, whereby pairing a mineral with an organic molecule helps it pass through the body easier.
-
🏭 High manufacturing standards: all of our supplements here at Supplement Needs are manufactured right here in the UK in accordance with Good Manufacturing Processes to ensure consistently excellent quality and safety.
-
🧑🎓 Expertly formulated: our supplements aren’t just formulated by anyone. Dr Dean St Mart PhD is involved at every step of the process, to ensure each ingredient has a beneficial function to support your health. What other brands can say the same?
If you’re looking for a female supplement that ticks all the boxes, then discover PMS+ from Supplement Needs today…
Support female health with Supplement Needs
For more insights and information about supplements, discover the Supplement Needs blog…
Why You Should Avoid Cheap Vitamins & Multivitamins | What You Should Look for in Pregnancy Supplements | The Importance of Sleep Hygiene
Disclaimer
The information on this website should not be used as a substitute for professional medical advice or care. If you have questions about your health, please contact your doctor.
References
1. Gudipally, P.R., & Sharma, G.K., 2023, ‘Premenstrual Syndrome’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560698/. Accessed on 29th September 2025.
2. NHS Online, 2024, ‘PMS (premenstrual syndrome)’. Available from: https://www.nhs.uk/conditions/pre-menstrual-syndrome/. Accessed on 29th September 2025.
3. Thiyagarajan, D.K., Basit, H., & Jeanmonod, R., 2024, ‘Physiology, Menstrual Cycle’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500020/. Accessed on 29th September 2025.
4. Monis, C.N., & Tetrokalashvili, M., 2022, ‘Proliferative and Follicular Phases of the Menstrual Cycle’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542229/. Accessed on 29th September 2025.
5. National Cancer Institute Online, ‘Ovarian follicle’. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/ovarian-follicle/. Accessed on 29th September 2025.
6. Reed, B.G., MD & Carr, B.R., MD, 2018, ‘The Normal Menstrual Cycle and the Control of Ovulation’, Endotext [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279054/. Accessed on 29th September 2025.
7. Monis, C.N., & Tetrokalashvili, M., 2022, ‘Proliferative and Follicular Phases of the Menstrual Cycle’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542229/. Accessed on 29th September 2025.
8. Holesh, J.E., Bass, A.N., & Lord, M., 2023, ‘Physiology, Ovulation’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441996/. Accessed on 29th September 2025.
9. Thiyagarajan, D.K., Basit, H., & Jeanmonod, R., 2024, ‘Physiology, Menstrual Cycle’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500020/. Accessed on 30th September 2025.
10. Cleveland Clinic Online, 2024, ‘Corpus Luteum’. Available from: https://my.clevelandclinic.org/health/body/21849-corpus-luteum. Accessed on 30th September 2025.
11. Oliver, R., & Pillarisetty, L.S., 2023, ‘Anatomy, Abdomen and Pelvis, Ovary Corpus Luteum’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/sites/books/NBK539704/. Accessed on 30th September 2025.
12. Thiyagarajan, D.K., Basit, H., & Jeanmonod, R., 2024, ‘Physiology, Menstrual Cycle’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500020/. Accessed on 30th September 2025.
13. NHS Online, 2023, ‘Periods and fertility in the menstrual cycle’. Available from: https://www.nhs.uk/conditions/periods/fertility-in-the-menstrual-cycle/. Accessed on 29th September 2025.
14. NHS Online, 2023, ‘Periods’. Available from: https://www.nhs.uk/conditions/periods/. Accessed on 30th September 2025.
15. Gudipally, P.R., & Sharma, G.K., 2023, ‘Premenstrual Syndrome’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560698/. Accessed on 30th September 2025.
16. Haufe, A., & Leeners, B., 2023, ‘Sleep Disturbances Across a Woman’s Lifespan: What is the Role of Reproductive Hormones?’, J Endocr Soc., 7(5):bvad036. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10117379/. Accessed on 30th September 2025.
17. NHS Online, 2024, ‘PMS (premenstrual syndrome)’. Available from: https://www.nhs.uk/conditions/pre-menstrual-syndrome/. Accessed on 29th September 2025.
18. Mind Charity Online, 2024, ‘Symptoms of premenstrual dysphoric disorder (PMDD)’. Available from: https://www.mind.org.uk/information-support/types-of-mental-health-problems/premenstrual-dysphoric-disorder-pmdd/symptoms-of-pmdd/. Accessed on 29th September 2025.
19. NHS Online, 2020, ‘B vitamins and folic acid’. Available from: https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-b/. Accessed on 30th September 2025.
20. Modzelewski, S., et al., 2024, ‘Premenstrual syndrome: new insights into etiology and review of treatment methods’, Front Psychiatry, 15. Available from: https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2024.1363875/full. Accessed on 30th September 2025.
21. Deutch, B., Jørgensen, E.B., & Hansen, J.C., 2000, ‘Menstrual discomfort in Danish women reduced by dietary supplements of omega-3 PUFA and B12 (fish oil or seal oil capsules)’, Nutrition Research, 20(5):621-631. Available from: https://www.sciencedirect.com/science/article/abs/pii/S0271531700001524. Accessed on 30th September 2025.
22. Sultana, A., 2022, ‘A Systematic Review and Meta-Analysis of Premenstrual Syndrome with Special Emphasis on Herbal Medicine and Nutritional Supplements’, Pharmaceuticals, 15(11):1371. Available from: https://www.mdpi.com/1424-8247/15/11/1371. Accessed on 30th September 2025.
23. HS Online, 2020, ‘Others: Vitamins and minerals’. Available from: https://www.nhs.uk/conditions/vitamins-and-minerals/others/. Accessed on 30th September 2025.
24. Siminiuc, R., & Țurcanu, D., 2023, ‘Impact of nutritional diet therapy on premenstrual syndrome’, Front Nutr., 10. Available from: https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1079417/full. Accessed on 30th September 2025.
25. NHS Online, 2020, ‘Vitamin D’. Available from: https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/. Accessed on 30th September 2025.
26. Siminiuc, R., & Țurcanu, D., 2023, ‘Impact of nutritional diet therapy on premenstrual syndrome’, Front Nutr., 10. Available from: https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2023.1079417/full. Accessed on 30th September 2025.
27. asan, A., et al., 2024, ‘Traditional herbal interventions for premenstrual syndrome management: A comprehensive literature review’, International Journal of Chemical and Biochemical Sciences, 25(18):120-140. Available from: https://www.researchgate.net/publication/378736891_Traditional_herbal_interventions_for_premenstrual_syndrome_management_A_comprehensive_literature_review. Accessed on 30th September 2025.
28. Cleveland Clinic Online, 2023, ‘Inositol’. Available from: https://my.clevelandclinic.org/health/drugs/25173-inositol. Accessed on 30th September 2025.
29. ibid.
30. Cantelmi, T., et al., 2021, ‘Inositol treatment for psychological symptoms in Polycystic Ovary Syndrome women’, Eur Rev Med Pharmacol Sci., 25:2383-2389. Available from: https://www.europeanreview.org/wp/wp-content/uploads/2383-2389.pdf. Accessed on 30th September 2025.
31. Khayat, S., et al., 2014, ‘Effect of Treatment with Ginger on the Severity of Premenstrual Syndrome Symptoms’, ISRN Obstet Gynecol., 2014:792708. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4040198/. Accessed on 30th September 2025.
32. ibid.
33. Nguyen, T., & Alzahrani, T., 2023, ‘Ginkgo Biloba’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541024/. Accessed on 30th September 2025.
34. Sultana, A., 2022, ‘A Systematic Review and Meta-Analysis of Premenstrual Syndrome with Special Emphasis on Herbal Medicine and Nutritional Supplements’, Pharmaceuticals, 15(11):1371. Available from: https://www.mdpi.com/1424-8247/15/11/1371. Accessed on 30th September 2025.
35. Drugs.com, 2025, ‘Chaste Tree’. Available from: https://www.drugs.com/npp/chaste-tree.html. Accessed on 30th September 2025.
36. Rafieian-Kopaei, M., & Movahedi, M., 2017, ‘Systematic Review of Premenstrual, Postmenstrual and Infertility Disorders of Vitex Agnus Castus’, Electron Physician., 9(1):3685-3689. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5308513/. Accessed on 30th September 2025.
37. Livertox [Internet], 2024, ‘Lemon Balm’. Available from: https://www.ncbi.nlm.nih.gov/books/NBK600583/. Accessed on 30th September 2025.
38. Mirabi, P., et al., 2018, ‘The Effects of Lemon balm on Menstrual Bleeding and the Systemic Manifestation of Dysmenorrhea’, Iran J Pharm Res., 17(Suppl2):214-223. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6447884/. Accessed on 30th September 2025.
39. Robinson, J., et al., 2024, ‘Effect of nutritional interventions on the psychological symptoms of premenstrual syndrome in women of reproductive age: a systematic review of randomized controlled trials’, Nutr Rev., 83(2):280-306. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11723155/. Accessed on 30th September 2025.