Thought to affect 1 in 10 women in the UK 1, PCOS is the most common condition associated with the endocrine (hormone) system in females of reproductive age2. But what actually is it? And how can you manage PCOS symptoms? Understanding these questions can make a huge difference to your quality of life if you are living with PCOS. With that in mind, we’ll explore everything you need to know about PCOS, including how to choose the best PCOS supplements to help you manage your symptoms…
What is PCOS?
PCOS stands for Polycystic Ovary Syndrome. It’s been discussed a lot in the media recently, as more and more research is being invested into understanding female health and conditions around fertility and endocrine function. And, despite the name, your ovaries don’t actually need to have cysts for you to have PCOS3. They can still be present4, but it is not a requirement for a diagnosis (as we will discuss later).
But, what is PCOS? In a nutshell, PCOS affects how ovaries work.
The ovary has two main purposes:
-
To produce and release a range of hormones, including oestrogen, testosterone, inhibin, and progesterone5. This activity increases after puberty, and fluctuates according to the phases of the menstrual cycle.
-
To house immature egg cells, called oocytes, which mature and are released during ovulation. Egg cells begin to develop while the foetus is still in the womb, and pause until puberty6.
In a regular ovary, the secretion of these hormones is largely consistent (with respect to the hormonal balances of each individual), and the ovary is able to release a new ovum, or egg, each menstrual cycle.
However, PCOS hinders the typical ovarian function. This can manifest in a range of symptoms due to the imbalance of hormones and non-release of new ova. Or, to put it another way, PCOS stops the ovary from working properly, which can have an impact on fertility and a wide range of other bodily functions.
PCOS symptoms
But how do you know if you have PCOS? For some, it can be completely asymptomatic, meaning some women don’t know that they have PCOS at all. However, it may be discovered if you have difficulties getting pregnant, or gaining weight without a clear explanation7.
For those who do experience symptoms, these can include8:
-
Intermittent, absent, or unpredictable menstruation: since PCOS affects the ovaries, and the release of eggs, abnormal or irregular periods are a common symptom. This can include unpredictable periods, no periods at all, or heavier bleeding during your period.
-
Hirsutism: this is where you have excess hair growth, and can be seen particularly on your arms, chest, abdomen and face with PCOS. Research suggests that around 65-75% of people with polycystic ovary syndrome experience excess hair growth9.
-
Hair loss: conversely, some may experience hair loss or thinning hair on the head. This is called androgenic alopecia 10, or female pattern baldness, and is thought to be due to elevated levels of androgens (which is common in PCOS).
-
Acne: acne is a common symptom of hormone imbalances, and people with PCOS may have acne on their face, chest, and back well after their teenage years. It may also be fairly difficult to treat and manage.
-
Obesity: according to recent studies, around 38-88% have obesity or are overweight 11. Weight management can be incredibly difficult for people with PCOS due to the links with insulin resistance, fat distribution, and metabolic function. Or, more simply, the way PCOS affects the body can also impact your ability to manage your blood sugar, burn energy after meals, and where the fat appears on the body.
-
Patches of skin darkening: skin darkening, called acanthosis nigricans 12, is associated with PCOS due to issues with insulin resistance and hyperandrogenism (a higher amount of androgens, which are sex hormones like testosterone).
-
Cysts: while not required for a diagnosis, some people may experience ovarian cysts, or ovaries that look larger than average on an ultrasound.
-
Infertility: with the irregular ovarian function and its impact on ovulation, PCOS is the leading cause of female infertility. Many struggle to get pregnant because of it.
Related conditions
Aside from the more immediate symptoms, PCOS is associated with an increased risk of developing certain long-term health conditions. These include 13:
-
Type 2 diabetes: the hormonal imbalances and increased likelihood of obesity that are typical of PCOS can lead to increased insulin resistance, which is where the body doesn’t respond to insulin properly. This means that PCOS can be considered a ‘pre-diabetic state’. Research suggests that around 50-80% of PCOS patients can develop insulin resistance, and that women with PCOS and obesity are eight times more likely to develop type 2 diabetes 14.
-
Depression, low mood, and mood swings: there is a lot of documentation of depression and anxiety amongst people with PCOS 15; depending on the studies, this percentage ranges from 16-55%. Whilst exact causes for this higher prevalence of depressive disorders is unclear, it could be due to the impact of symptoms on quality of lift, hormonal imbalances, or a combination thereof.
-
Hypertension and high cholesterol: people with PCOS are more at risk of developing hypertension (high blood pressure) and elevated cholesterol, potentially due to 16:
-
Hyperalderosteronism: an overproduction of aldosterone, which is involved in regulating blood pressure.
-
Insulin resistance and increased blood insulin levels: higher levels of blood insulin can cause your body to absorb too much salt, or affect vasodilation (which is when your blood vessels expand and contract with blood flow).
-
Hyperandrogenism: increased levels of androgens can impact blood pressure.
-
Dyslipidaemia: this is where you have higher than average levels of fat in your bloodstream, which can damage blood vessel walls, consolidate into cholesterol deposits, and make your heart work harder to pump blood.
-
Cardiovascular disease and strokes: an increase in the above conditions also increases your chances of developing heart disease, as your heart is overworking to pump blood around the body. Chances of ischaemic strokes, which are caused by blockages or the narrowing and hardening of blood vessels (depriving the brain of oxygen), can also become more of a risk.
-
Sleep apnoea: obesity can lead to the development of sleep apnoea, which is where your breathing stops and starts when you sleep 17.
People with PCOS can also have a higher chance of developing endometrial cancer (of the womb lining) due to the absence of their periods. Alongside the fertility issues, there is some evidence that PCOS may also increase the risk of pregnancy complications and miscarriage 18.
Diagnosis of Polycystic Ovary Syndrome
Of course, identifying symptoms is only one step in the process; the next is to get a diagnosis. PCOS is considered a ‘diagnosis of exclusion’, since the symptoms can implicate a range of endocrine or ovulatory disorders. In order to make a diagnosis, doctors will look to exclude other conditions, such as irregular thyroid function or hyperprolactinemia, to help understand what is happening to your body 19.
For a diagnosis of polycystic ovary syndrome, the prevailing guidance suggests that doctors look for at least two of the following criteria20.
-
Irregular or infrequent periods. This indicates that there could be something happening with your ovaries, where ovulation is not occurring as it should.
-
High levels of clinical or biochemical androgens like testosterone shown in a blood test. Other symptoms of excess androgens, as mentioned above, may be taken as an indication, even with a normal blood test.
-
Polycystic ovaries seen on an ultrasound.
What are the causes of PCOS?
The exact cause for PCOS is unknown. However, research suggests that both genetic and environmental factors can play a part in developing the condition.
For example, PCOS symptoms have been seen to run in families, which suggests that some people have a genetic disposition to PCOS. Scientists have found a potential of 19 different genetic changes that could cause PCOS, which may explain just why polycystic ovary syndrome exhibits such a variation of symptoms from person to person21.
The different types of PCOS
Polycystic ovary syndrome is not the same for everyone. In fact, depending on the symptoms, PCOS can be split into different ‘types’.2223
Classic phenotype PCOS
Classic phenotype PCOS is categorised by “significant symptoms associated with menstrual dysfunction, hyperinsulinemia, insulin resistance, and increased risk of metabolic syndrome”.
Effectively, this means that classic PCOS is concerned with irregular periods, elevated blood insulin, and symptoms that can increase your risk of longer-term conditions like heart disease. People with this type of PCOS can also have a higher risk of obesity and elevated blood fat levels.
Classic phenotype can be further divided into Phenotypes A and B; A is the most common, and is characterised by excess androgen, irregular ovulation, and polycystic ovaries; while someone with Phenotype B may present with excess androgen and dysfunctional ovulation, but no visible cysts on their ovaries.
Ovulatory PCOS
Also known as Phenotype C, ovulatory PCOS is primarily characterised by excess androgen production and polycystic ovaries. It is distinct from other types, as ovulation can and does still occur. This not only reduces complications related to fertility, but also means people with this type of PCOS still have regular periods. Instead, their symptoms could be more related to excess hair growth.
Non-hyperandrogenic PCOS
Lastly, Phenotype D is referred to as non-hyperandrogenic PCOS as patients can experience issues with ovulation and have polycystic ovaries, without elevated levels of androgens detected in the blood.
This means that you may have primarily regular periods, with occasional irregularities. In addition, your day-to-day symptoms may be fairly mild, as you do not have the same hormonal imbalance as other forms of PCOS.
PCOS treatments
We’re going to come right out and say it. In conventional Western medicine, there is currently no recognised “cure” for PCOS.
That said, many experts emphasise that symptoms often have underlying causes which can be addressed. Through lifestyle changes and targeted management strategies, it is possible for many women to reduce or even reverse the impact of symptoms.
While no single approach works for everyone, the most common treatment options for polycystic ovary syndrome include:
Lifestyle changes
It’s often repeated ad nauseam, but maintaining a healthy diet, getting regular exercise, and staying around a healthy weight (for your body) can make a big difference to how you feel, how you move, and your overall health.
This is especially true for PCOS, as losing even just 5% of your body weight has been seen to greatly improve PCOS symptoms24. Exercising and eating well is also important for reducing the risk of long-term conditions like hypertension, high cholesterol, and cardiovascular disease.
Depending on your symptoms, adding supplements for PCOS into your diet can help you to improve and manage your symptoms (as you’ll see below).
Prescribed medicines
Depending on your lifestyle, there are a range of medicines that can help you to manage your symptoms25.
For example, if you’re not looking to get pregnant, the contraceptive pill may help you to have more regular periods. The addition of extra proestins to your system can help your body to shed the uterine lining regularly and support uterine health. Other hormonal contraceptives are an option, such as the intrauterine device (IUD), to help keep the uterine lining thin without necessarily resulting in a period.
Disclaimer: while hormonal birth control (HBC) can help reduce androgen levels in many women, it also suppresses ovulation. As a result, it is often regarded as a temporary measure that does not address the underlying cause.
If you are hoping to get pregnant, there are some medications you may be prescribed.
-
Clomifene is used to encourage your ovaries to release an egg for conception.
-
If Clomifene doesn’t work for you, you may be prescribed Metformin. This can help to stimulate ovulation and regular periods, while also lowering your insulin levels in the blood.
Note: according to the NHS, “Metformin is not licensed for treating PCOS in the UK” but “it can be used ‘off-label’ in certain circumstances”26. Off-label is used to describe the use of a licensed medicine for treating conditions outside the drug company’s licence. This does not mean that it is unsafe, but that it is not an advertised use. Your medical professional should only prescribe off-label medicines after careful consideration of all options available.
The combined contraceptive pill can also help to treat excessive hair growth, or hair loss. Alternatively, you may be prescribed anti-androgen medicines, such as flutamide, cyproterone acetate, or spironolactone to help manage excess hair growth.
Fertility treatments
If you are struggling to conceive with PCOS, and lifestyle interventions or pharmaceutical support have not helped, you may be offered the chance to use IVF. This is where eggs are removed, fertilised outside the womb, and implanted back into the womb.
You may also be eligible for a minor surgical procedure called laparoscopic ovarian drilling (LOD) to try and correct the hormone imbalance and restore regular ovarian function.
The best supplements to manage and support PCOS symptoms
As we said above, there are several supplement ingredients that can help you to manage your PCOS symptoms. But, how do you know what to look for? Below, we’ve explored some of the best PCOS supplements, and highlighted the ingredients you should look out for to support your health.
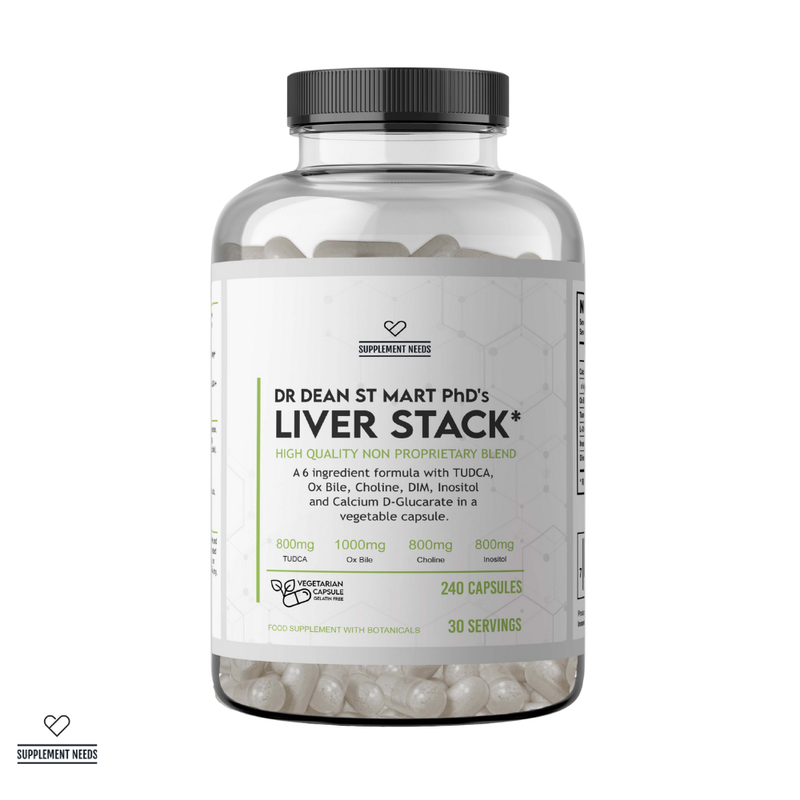
PCOS-specific supplements

There are a wide range of female-specific supplements on the market. But how many are explicitly tailored to help with PCOS symptoms? Rather than having a collection of different tablets you need to take, you should look for supplements which have included the best ingredients into one easy tablet.
At Supplement Needs, we’ve gone above and beyond to offer you the best PCOS supplements to support your health and manage your symptoms. We’ve also only chosen the best form of each ingredient for superior quality and absorption. In our PCOS+ Capsules, you can find:
-
Myo-inositol: according to research, myo-inositol has a very positive impact on regulating the menstrual cycle and lowering insulin levels, with only minor side effects27. This makes it a great option for PCOS treatment.
-
D-Chiro Inositol: used in a 40:1 ratio, myo-inositol and D-Chiro Inositol has shown to help support healthy ovarian function28.
-
Thiamine tetrahydrofurfuryl disulfide: Thiamine, or Vitamin B1, has been shown to have a potentially favourable effect on improving general health and fertility outcomes for women with polycystic ovary syndrome29. We’ve used thiamine tetrahydrofurfuryl disulfide, which is the most bioavailable form of the vitamin, for enhanced absorption.
-
Cinnulin Cinnamon: while there is scope for more research, preliminary studies have found that cinnamon may help to improve insulin resistance30, which is a common factor in PCOS.
-
CurcuPrime (Tetrahydrocurcumin): well-known for being an anti-inflammatory, antioxidant, and anti-hyperlipidemic, curcumin has significant promise as a treatment for PCOS. Research shows that these qualities, along with its ability to reduce insulin resistance, may help to alleviate PCOS symptoms31.
-
Licorice Dry Extract Glycyrrhiza glabra: early research suggests that licorice may help to reduce blood insulin levels, blood cholesterol levels, and insulin resistance32.
-
NAC: NAC, or N-acetylcysteine, is a valuable antioxidant and insulin-sensitiser. Research suggests this can help to improve progesterone levels and endometrial thickness (the lining of the uterus), which may be a potential treatment option for fertility33.
-
Quercetin Dihydrate: current research suggests that quercetin may be a promising treatment for PCOS, helping to improve fertility, while reducing hormonal imbalances, insulin resistance, excess androgen production and more34.
-
Pycrinil Artichoke: artichoke extract has been linked with improving inflammation and helping to reduce the effects of lipid metabolism disorders35 (aka how the body processes fats).
-
Calcium Butyrate: butyrate has been shown to aid the restoration of hormonal balance, enhance insulin sensitivity, and reduce chronic inflammation that can happen with PCOS36.
Additional supplements to manage PCOS symptoms
Outside of specific PCOS supplements, there are some ingredients that have shown to have a beneficial impact on symptoms. These include:
-
Vitamin D: Vitamin D is a great all-rounder to support your health. As a PCOS supplement, studies show that Vitamin D can help improve periods, improve the maturation of eggs in the ovary (folliculogenesis), and decrease blood testosterone levels: all of which may help to improve fertility outcomes37.
-
Zinc: when it comes to quality of life, zinc has been shown to help reduce menstrual pain and reduce insulin resistance38.
-
Glutathione: Glutathione is important for binding insulin into the cells (and therefore glucose uptake). In PCOS, where insulin resistance is a common issue, supplementary Glutathione may help to reduce blood insulin levels and alleviate related symptoms39.
Choosing the best PCOS supplements
Support your health with supplements explicitly formulated to work with (and for) the female body. At Supplement Needs, our exclusive Female Range has been diligently crafted by Dr. Dean St Mart PhD, offering you the perfect balance of science and dedicated research that is expertly tailored to support and nourish female health.
There are several key qualities you need to look out for when you’re choosing the best PCOS supplements, and at Supplement Needs we hit them all:
-
♀️ Contains an efficacious blend of ingredients to support and empower female health.
-
🍀 Contains ingredients in their bioavailable, highly-absorbable form where possible.
-
💪 Uses non-generic, high-quality ingredients for superior quality.
-
🎓 Developed by credentialed experts, like Dr Dean St Mart.
-
🏭 Manufactured to GMP and ISO guidelines.
-
👩 Created by people who care about supporting your health.
Discover the Female Needs range today
For more insights and the latest information about supplements, discover the Supplement Needs blog…
Why You Should Avoid Cheap Vitamins & Multivitamins | The Best Supplements for PMS: The Supplement Needs Guide | What You Should Look for in Pregnancy Supplements
Disclaimer
The information on this website should not be used as a substitute for professional medical advice or care. If you have questions about your health, please contact your doctor.
References
1. NHS Online, 2022, ‘Polycystic Ovary Syndrome: Overview’. Available from https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/. Accessed on 30th October 2025.
2. Shukla, A., Rasquin, L.I., Anastasopoulou, C., 2025, ‘Polycystic Ovarian Syndrome’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459251/. Accessed on 30th October 2025
3. NHS Online, 2022, ‘Polycystic Ovary Syndrome: Overview’. Available from https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/. Accessed on 30th October 2025.
4. Mobeen, S., & Apostol, R., 2023, ‘Ovarian Cyst’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560541/. Accessed on 31st October 2025.
5. Gibson, E., & Mahdy, H., 2023, ‘Anatomy, Abdomen and Pelvis, Ovary’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545187/. Accessed on 31st October 2025.
6. ibid.
7. Cleveland Clinic Online, 2023, ‘Polycystic Ovary Syndrome (PCOS)’. Available from: https://my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos. Accessed on 31st October 2025.
8. ibid.
9. Spritzer, P.M., et al., 2022, ‘Hirsutism, Normal Androgens and Diagnosis of PCOS’, Diagnostics (Basel), 12(8):1922. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9406611/. Accessed on 4th November 2025.
10. Quinn, M., et al., 2014, ‘Prevalence of androgenic alopecia in patients with polycystic ovary syndrome and characterization of associated clinical and biochemical features’, Fertil Steril., 101(4): 1129-34. Available from: https://pubmed.ncbi.nlm.nih.gov/24534277/. Accessed on 4th November 2025.
11. Barber, T., et al., 2019, ‘Obesity and Polycystic Ovary Syndrome: Implications for Pathogenesis and Novel Management Strategies’, Clin Med Insights Reprod Health., 13:1179558119874042. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6734597/. Accessed on 4th November 2025.
12. Hughes, E.K., Brady, M.F., & Rawla, P., 2023, ‘Acanthosis Nigricans’, StatPearls [Internet]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431057/. Accessed on 4th November 2025.
13. NHS Online, 2022, ‘Polycystic Ovary Syndrome: Symptoms’. Available from: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/symptoms/. Accessed on 4th November 2025.
14. Agrawal IV, A., Dave, A., & Jaiswal, A., 2023, ‘Type 2 Diabetes Mellitus in Patients With Polycystic Ovary Syndrome’, Cureus, 15(10):e46859. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10637759/. Accessed on 4th November 2025.
15. Dybciak, P., et al., 2023, ‘Depression in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis’, J Clin Med., 12(20):6446. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10607337/. Accessed on 4th November 2025.
16. Kovell, L.C., Juraschek, S.P., & Michos, E.D., 2021, ‘Hypertension in Young Women: Implications of the Polycystic Ovary Syndrome and Opportunities for Prevention and Further Research’, J Clin Endocrinol Metab., 106(9): e3775-e3777. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8372631/. Accessed on 4th November 2025.
17. NHS Online, 2022, ‘Sleep Apnoea’. Available from: https://www.nhs.uk/conditions/sleep-apnoea/. Accessed on 4th November 2025.
18. Bui, L.M., et al., 2024, ‘Polycystic ovary syndrome and miscarriage: a narrative review’, F&S Reviews, 5(4):100078. Available from: https://www.sciencedirect.com/science/article/abs/pii/S2666571924000355. Accessed on 4th November 2025.
19. Islam, H., et al., 2022, ‘An update on polycystic ovary syndrome: A review of the current state of knowledge in diagnosis, genetic etiology, and emerging treatment options’, Womens Health (Lond), 18:17455057221117966. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9386861/. Accessed on 4th November 2025.
20. NHS Online, 2022, ‘Polycystic Ovary Syndrome: Diagnosis’. Available at: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/diagnosis/. Accessed on 4th November 2025.
21. National Institute of Child Health and Human Development Online, 2024, ‘What causes PCOS?’. Available from: https://www.nichd.nih.gov/health/topics/pcos/conditioninfo/causes. Accessed on 4th November 2025.
22. Nautiyal, H., et al., 2022, ‘Polycystic Ovarian Syndrome: A Complex Disease with a Genetics Approach’, Biomedicines, 10(3):540. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8945152/. Accessed on 4th November 2025.
23. Sachdeva, G., et al., 2019, Comparison of the Different PCOS Phenotypes Based on Clinical Metabolic, and Hormonal Profile, and their Response to Clomiphene’, Indian J Endocrinol Metab., 23(3):326–331. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6683693/. Accessed on 4th November 2025.
24. NHS Online, 2022, ‘Polycystic Ovary Syndrome: Treatment’. Available from: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/treatment/. Accessed on 4th November 2025.
25. ibid.
26. ibid.
27. Sharon, P.M., et al., 2024, ‘The Effectiveness of Myo-Inositol in Women With Polycystic Ovary Syndrome: A Prospective Clinical Study’, Cureus, 16(2):e53951. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10926319/. Accessed on 4th November 2025.
28. Facchinetti, F., et al., 2020, ‘Inositols in Polycystic Ovary Syndrome: An Overview on the Advances’, Trends Endocrinol Metab., 31(6):435-447. Available from: https://pubmed.ncbi.nlm.nih.gov/32396844/. Accessed on 4th November 2025.
29. Moti, M., et al., 2024, ‘The Effects of Thiamine Supplementation on General Health and Infertility Treatment Outcomes in Women with Polycystic Ovary Syndrome: A Triple-Blinded Randomized Placebo-Controlled Clinical Trial’, Int J Fertil Steril., 18(2):128-134. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10875311/. Accessed on 4th November 2025.
30. Dou, L., et al., 2018, ‘The effect of cinnamon on polycystic ovary syndrome in a mouse model’, Reprod Biol Endocrinol., 16:99. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6194596/. Accessed on 4th November 2025.
31. Mallya, P., & Lewis, S.A., 2025, ‘Curcumin and its formulations for the treatment of polycystic ovary syndrome: current insights and future prospects’, Journal of Ovarian Research, 18(78). Available from: https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01660-z. Accessed on 4th November 2025.
32. Hooshmandi, H., et al., 2024, ‘Effects of licorice extract in combination with a low-calorie diet on obesity indices, glycemic indices, and lipid profiles in overweight/obese women with polycystic ovary syndrome (PCOS): a randomized, double-blind, placebo-controlled trial’, Journal of Ovarian Research, 17(157). Available from: https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-024-01446-9. Accessed on 4th November 2025.
33. Viña, I., et al., 2025, ‘Efficacy of N-Acetylcysteine in Polycystic Ovary Syndrome: Systematic Review and Meta-Analysis’, Nutrients, 17(2):284. Available from: https://pubmed.ncbi.nlm.nih.gov/39861414/. Accessed on 4th November 2025.
34. Habiburrahman, M., et al., 2023, ‘Quercetin as a noteworthy treatment for polycystic ovary syndrome: An evidence-based review from molecular basis mechanism to clinical perspective’, Obesity Medicine, 39:100490. Available from: https://www.sciencedirect.com/science/article/abs/pii/S2451847623000143. Accessed on 4th November 2025.
35. Szczuko, M., et al., 2021, ‘Nutrition Strategy and Life Style in Polycystic Ovary Syndrome—Narrative Review’, Nutrients, 13(7):2452. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8308732/. Accessed on 4th November 2025.
36. Kim, N., & Yang, C., 2024, ‘Butyrate as a Potential Modulator in Gynecological Disease Progression’, Nutrients, 16(23):4196. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11644728/. Accessed on 4th November 2025.
37. Mohan, A., et al., 2023, ‘Vitamin D and polycystic ovary syndrome (PCOS): a review’, Ann Med Surg (Lond)., 85(7):3506-3511. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC10328709/. Accessed on 4th November 2025.
38. Nasiadek, M., et al., 2020, ‘The Role of Zinc in Selected Female Reproductive System Disorders’, Nutrients, 12(8):2464. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7468694/. Accessed on 4th November 2025.
39. Sandhu, J.K., et al., 2021, ‘Oxidative Stress in Polycystic Ovarian Syndrome and the Effect of Antioxidant N-Acetylcysteine on Ovulation and Pregnancy Rate’, Cureus., 13(9):e17887. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8502752/. Accessed on 4th November 2025.